标签:
HBV 表明抗原阳性是HCC最重要风险因子
Seropositivity for the hepatitis B surface antigen (HBsAg) is one of the most important risk factors for hepatocellular carcinoma
hbv e 抗原阳性会增加HCC风险
In our previous study, seropositivity for the hepatitis B e antigen (HBeAg) was associated with an increased risk for hepatocellular carcinoma.
The increased hepatocellular carcinoma risk in individuals seropositive for HBeAg remained significant regardless of serum level of alanine aminotransferase (ALT) and status of liver cirrhosis.8,9
serum HBV DNA level is used as a criterion for antiviral treatment in patients with chronic hepatitis B. Effective suppression of serum HBV DNA is a marker of efficacy for antiviral therapy
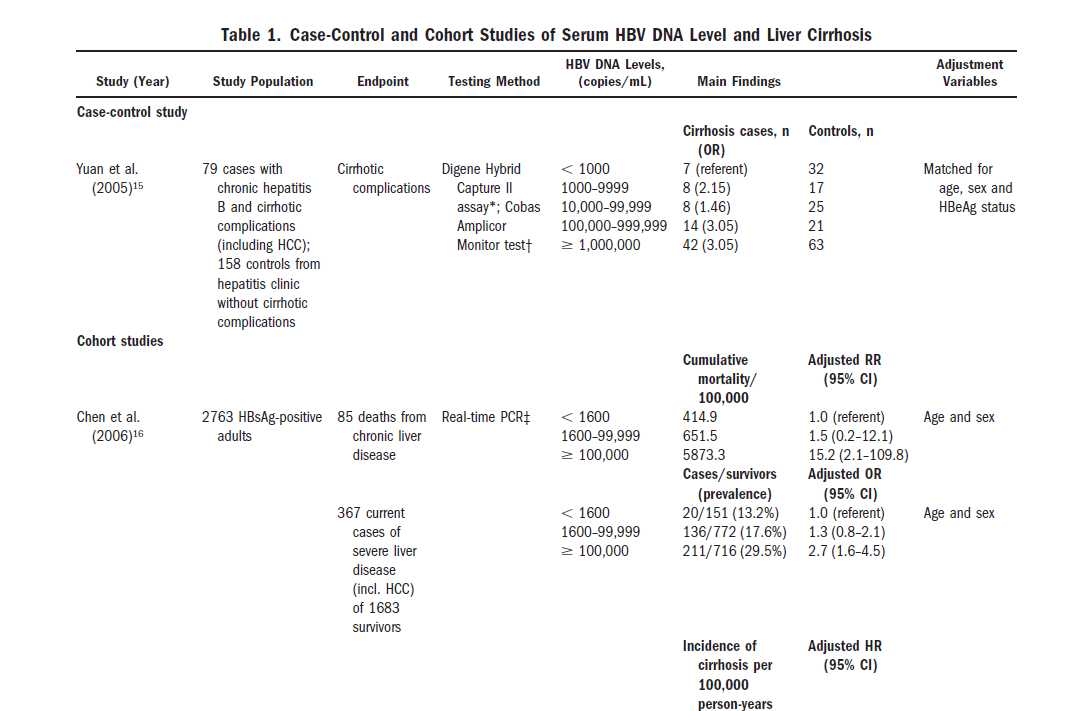
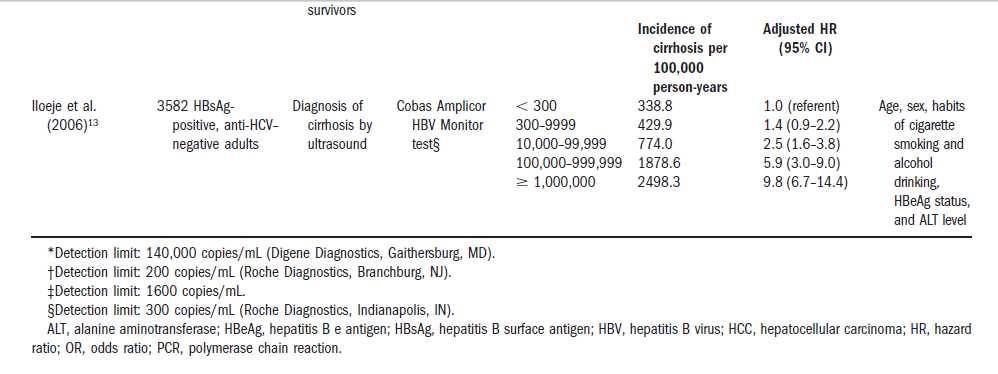
多变量回归分析肝癌的风险预测因子,逐渐增加的HBV DNA水平是最强的独立预测因子。
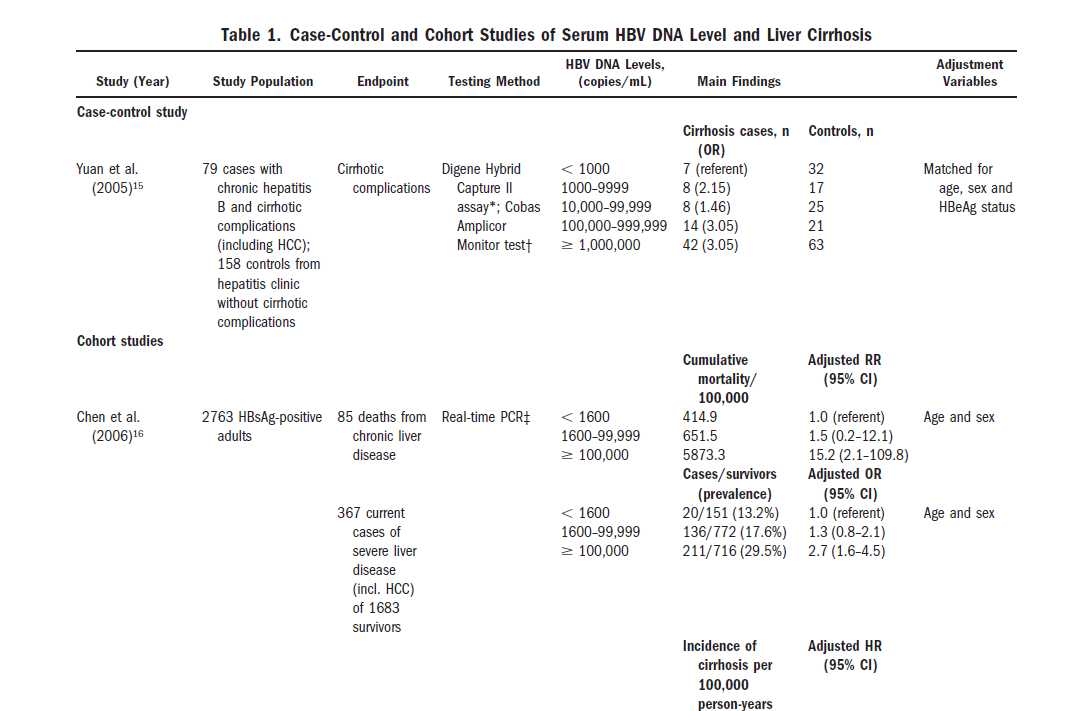
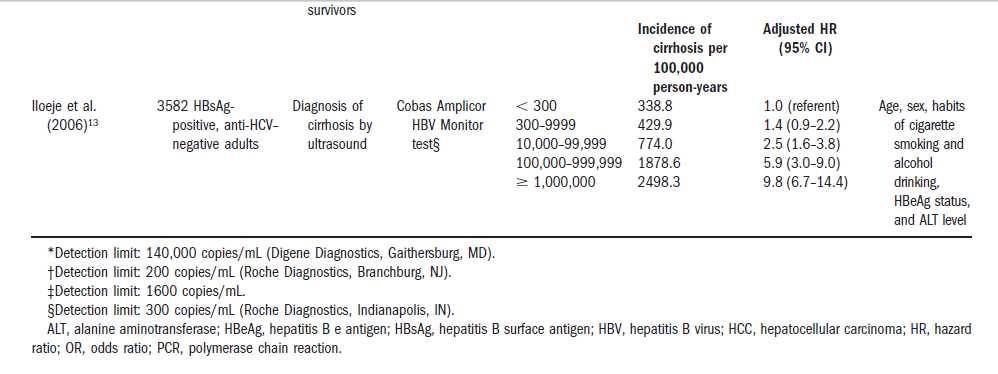
In multivariate Cox regression analyses
of risk factors predicting progression to liver cirrhosis,
increasing HBV DNA level was the strongest independent
predictor.
DNA复制程度的大小并不代表肝脏实际损害的程度,DNA复制程度高,并非就代表损害严重。
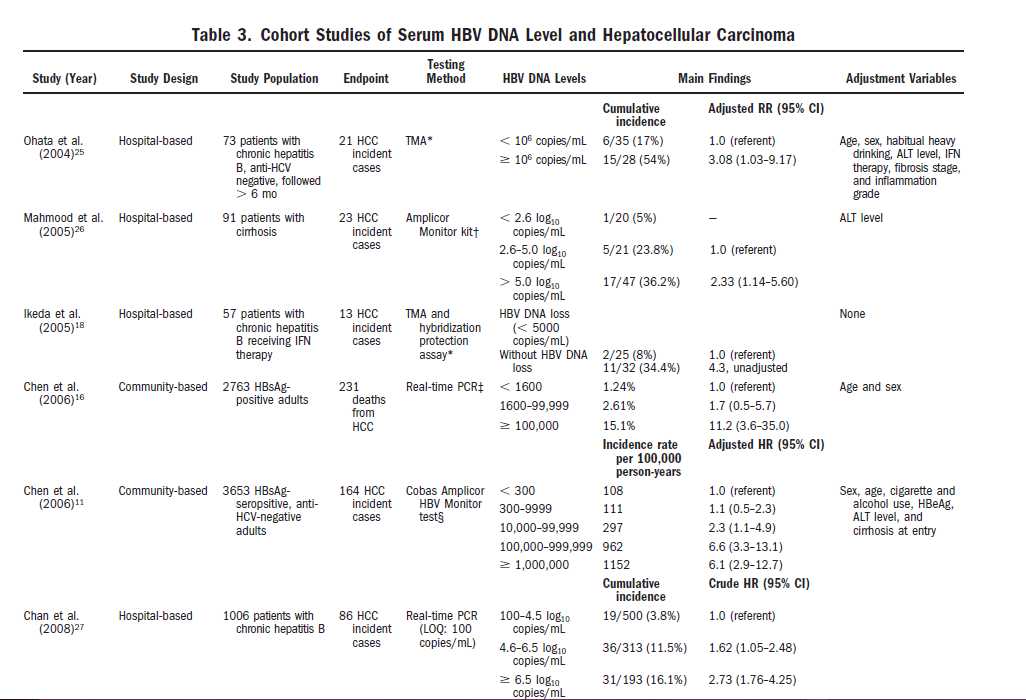
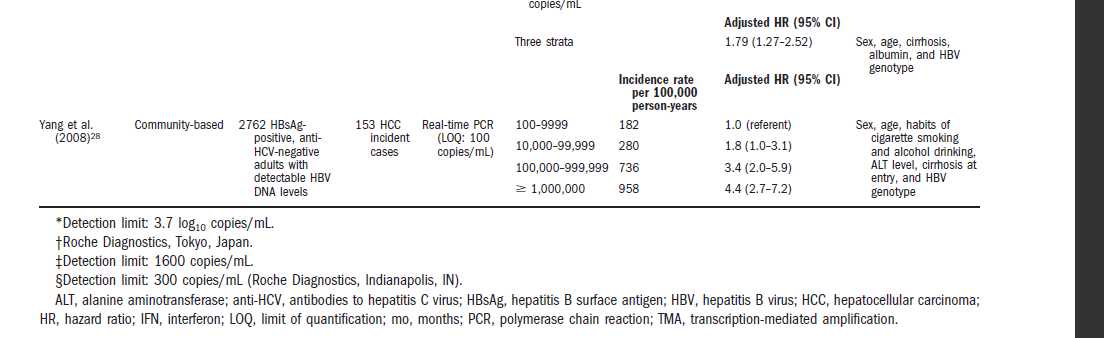
patients with HCC had higher
serum HBV DNA levels at study entry than patients with
cirrhosis who remained HCC-free during follow-up
The findings of cohort studies on the association between
serum HBV DNA levels and HCC risk are summarized
in Table 3.
血液中hbv DNA减少,肝脏得到极大改善
More importantly, improvement in histological
grade was strongly correlated with a decrease in serum
HBV DNA levels (r � 0.96; P � 0.001).
In four caseseries
studies on the recurrence of HCC after surgical resection34,38,39
or transarterial chemolipidolization,37 patients
with high serum HBV DNA levels at study entry had a
significantly higher risk of HCC recurrence than those with
low levels.
In multivariate Cox regression
analyses of risk factors predicting progression to mortality,
increasing HBV DNA level was the strongest
independent predictor of death from chronic liver disease
and cirrhosis, and was second to cirrhosis in predicting
death from HCC. There was no association between serum
HBV DNA levels and non–liver related mortality.
Recent unpublished data from this study, using
data on serum HBV DNA and ALT levels at multiple
time points and time-dependent regression modeling,
confirm that elevated serum HBV DNA at multiple time
points is indeed a very strong independent predictor of
HCC risk.44
http://www.ncbi.nlm.nih.gov/pubmed/23094699
HCC 风险因素:男性,年龄增大,转氨酶升高,HBV e抗原阳性,HBV-DNA偏高,HBV 的C段基因感染,核心基因变异
. In this community-based cohort study, male gender, older age, high serum alanine aminotransferase level, positive hepatitis B e antigen, higher HBV-DNA level, HBV genotype C infection, and core promoter mutation are independently associated with a higher risk of HCC.
While HBV-DNA level had better predictive accuracy than HBsAg level, when investigating the overall cohort in patients with HBV-DNA level < 2000 IU/mL, HBsAg level ≥ 1000 IU/mL was identified as a new independent risk factor for HCC
DNA指的是脱氧核糖核酸,病毒的复制是靠DNA的复制来完成的,DNA的浓度越高,病毒的复制越活跃。合起来,HBV-DNA指的就是乙肝病毒的脱氧核糖核酸。乙肝病毒DNA检测是判断乙肝病毒复制的常用手段。一般的,把数值大于10的3次方为阳性,把3-5次方认为是低量复制,5-7为中等量,大于7次方为大量。乙肝两对半并不能准确的判断病毒复制情况,DNA弥补了这个的不足。不过由于DNA检测技术要求严格,容易受到干扰,因此,一次结果不足以说明问题,遇到阳性,可以换医院再次检查。
DNA检测
编辑
以往乙肝患者抗病毒治疗的指征是:乙肝病毒e抗原阳性(大三阳)患者 HBVDNA数值要求达到10的5次方拷贝/毫升(20000U/ml),乙肝病毒e抗原阴性(小三阳)患者乙肝病毒DNA数值要求达到10的4次方拷贝 /毫升(2000U/ml),但是10的4次方拷贝/毫升以下也不能认为就没有问题了,最新的国际研究资料表明:和肝脏疾病进展相关的病毒DNA水平域值 尚不清楚,即使HBVDNA水平持续低于20000U/ml,也可能乙肝病毒情仍在进一步发展,因此HBVDNA数值应该越低越好,目前国际建议的 HBVDNA检测正常值应该是:< 50U/ml
5、其他:乙肝病毒DNA检测结果在一定程度上可以辅助判断乙肝病毒是否产生了变异,如在治疗过程中乙肝病毒dna检测结果由阴性转为阳性时,则提示病毒已发生变异,应结合具体病情重新选择抗病毒药物。
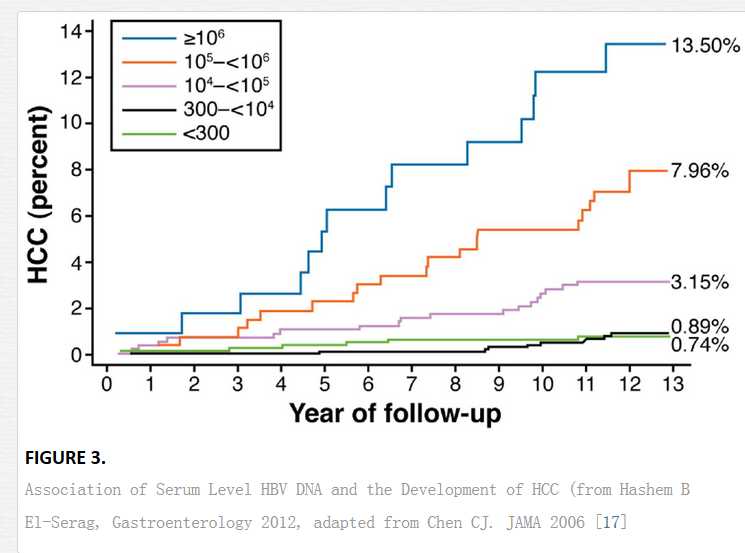
Participants with persistent elevation of serum HBV DNA level during follow-up had the highest hepatocellular carcinoma risk.
Conclusion Elevated serum HBV DNA level (≥10 000 copies/mL) is a strong risk predictor of hepatocellular carcinoma independent of HBeAg, serum alanine aminotransferase level, and liver cirrhosis
Context Serum hepatitis B virus (HBV) DNA level is a marker of viral replication and efficacy of antiviral treatment in individuals with chronic hepatitis B.
Objective To evaluate the relationship between serum HBV DNA level and risk of hepatocellular carcinoma.
Design, Setting, and Participants Prospective cohort study of 3653 participants (aged 30-65 years), who were seropositive for the hepatitis B surface antigen and seronegative for antibodies against the hepatitis C virus, recruited to a community-based cancer screening program in Taiwan between 1991 and 1992.
Main Outcome Measure Incidence of hepatocellular carcinoma during follow-up examination and by data linkage with the national cancer registry and the death certification systems.
Results There were 164 incident cases of hepatocellular carcinoma and 346 deaths during a mean follow-up of 11.4 years and 41 779 person-years of follow-up. The incidence of hepatocellular carcinoma increased with serum HBV DNA level at study entry in a dose-response relationship ranging from 108 per 100 000 person-years for an HBV DNA level of less than 300 copies/mL to 1152 per 100 000 person-years for an HBV DNA level of 1 million copies/mL or greater. The corresponding cumulative incidence rates of hepatocellular carcinoma were 1.3% and 14.9%, respectively. The biological gradient of hepatocellular carcinoma by serum HBV DNA levels remained significant (P<.001) after adjustment for sex, age, cigarette smoking, alcohol consumption, serostatus for the hepatitis B e antigen (HBeAg), serum alanine aminotransferase level, and liver cirrhosis at study entry. The dose-response relationship was most prominent for participants who were seronegative for HBeAg with normal serum alanine aminotransferase levels and no liver cirrhosis at study entry. Participants with persistent elevation of serum HBV DNA level during follow-up had the highest hepatocellular carcinoma risk.
Conclusion Elevated serum HBV DNA level (≥10 000 copies/mL) is a strong risk predictor of hepatocellular carcinoma independent of HBeAg, serum alanine aminotransferase level, and liver cirrhosis.
More than 350 million persons in the world are infected with chronic hepatitis B virus (HBV).1 It is particularly endemic in Taiwan, where the infection is usually acquired perinatally or in early childhood.2 Individuals with chronic hepatitis B infection are at an increased risk of developing liver cirrhosis, hepatic decompensation, and hepatocellular carcinoma3; 15% to 40% of these individuals will develop these serious sequelae during their lifetime.3,4 Hepatitis B virus is not directly cytopathic, and the development of hepatocellular carcinoma in individuals with chronic hepatitis B is a multistage, multifactorial process including the interaction between host and environmental factors.5 Risk factors for chronic HBV-related hepatocellular carcinoma include sex, age, cigarette smoking, alcohol consumption, chemical carcinogens, hormonal factors, and genetic susceptibility.6
Seropositivity for the hepatitis B surface antigen (HBsAg) is one of the most important risk factors for hepatocellular carcinoma.6 The risk of hepatocellular carcinoma associated with seropositivity for HBsAg ranges from 5-fold to 98-fold with a population-attributable risk of 8% to 94%.6 In our previous study, seropositivity for the hepatitis B e antigen (HBeAg) was associated with an increased risk for hepatocellular carcinoma.7 The adjusted hazard ratio (HR) of developing hepatocellular carcinoma was 9.6 for individuals seropositive for HBsAg and 60.2 for those seropositive for both HBsAg and HBeAg compared with those seronegative for both HBsAg and HBeAg. The increased hepatocellular carcinoma risk in individuals seropositive for HBeAg remained significant regardless of serum level of alanine aminotransferase (ALT) and status of liver cirrhosis.8,9
Highly sensitive testing methods based on polymerase chain reaction have become available for measuring serum level of HBV DNA. In current clinical practice guidelines,10- 13 serum HBV DNA level is used as a criterion for antiviral treatment in patients with chronic hepatitis B. Effective suppression of serum HBV DNA is a marker of efficacy for antiviral therapy.14 Its implementation as the primary surrogate end point instead of liver histology in assessment of new antiviral therapies remains to be validated.15 There are no long-term follow-up data on the relationship between serum HBV DNA level and risk of liver complications. In a small nested case-control analysis,7 we reported a significant association between serum HBV DNA level at study entry and hepatocellular carcinoma risk among individuals seronegative for HBeAg. However, there were only a small number of hepatocellular carcinoma cases and controls included in this study. Neither hepatocellular carcinoma incidence nor change in serum HBV DNA level over time was studied.
In this population-based, long-term prospective study, we followed up a total of 3653 individuals who were seropositive for HBsAg and seronegative for antibodies against hepatitis C virus (anti-HCV) at study entry. The goals of this study were to assess the biological gradient of hepatocellular carcinoma risk by (1) serum HBV DNA levels at study entry and adjusted for other risk factors including age, sex, cigarette smoking, alcohol consumption, seropositivity for HBeAg, elevated serum ALT level, and presence of liver cirrhosis at study entry; and (2) persistent elevation of serum HBV DNA level at both study entry and follow-up examinations.
Risk stratification for hepatitis B virus related hepatocellular carcinoma.
Abstract
Hepatitis B virus (HBV) infection is the major cause of chronic hepatitis, cirrhosis, and hepatocellular carcinoma (HCC) worldwide, especially in the Asia-Pacific region. Several hepatitis B viral factors predictive of clinical outcomes in HBV carriers have been identified. The Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer-HBV (REVEAL-HBV) study from Taiwan illustrated the strong association between HBV-DNA level at study entry and risk of HCC over time. In this community-based cohort study, male gender, older age, high serum alanine aminotransferase level, positive hepatitis B e antigen, higher HBV-DNA level, HBV genotype C infection, and core promoter mutation are independently associated with a higher risk of HCC. Another large hospital-based Elucidation of Risk Factors for Disease Control or Advancement in Taiwanese Hepatitis B Carriers cohort of Taiwanese patients further validated the findings of REVEAL-HBV. The risk of HCC started to increase when HBV-DNA level was higher than 2000 IU/mL. Both HBV-DNA and HBsAg levels were shown to be associated with HCC development. While HBV-DNA level had better predictive accuracy than HBsAg level, when investigating the overall cohort in patients with HBV-DNA level < 2000 IU/mL, HBsAg level ≥ 1000 IU/mL was identified as a new independent risk factor for HCC. With the results from REVEAL-HBV, a risk calculation for predicting HCC in non-cirrhotic patients has been developed and validated by independent cohorts (Risk Estimation for Hepatocellular Carcinoma in Chronic Hepatitis B).Taken together, ample evidence indicates that HBsAg level can complement HBV-DNA level in predicting HCC development, especially in HBV carriers with low viral load. In conclusion, HBV treatment guidelines should include the risk stratification of HCC to individualize the management of HBV carriers with different levels of HCC risk.
© 2012 Journal of Gastroenterology and Hepatology Foundation and Wiley Publishing Asia Pty Ltd.
http://www.intechopen.com/books/liver-tumors-epidemiology-diagnosis-prevention-and-treatment/epidemiology-and-risk-factors
HBV DNA level _data analysis
标签:
原文地址:http://www.cnblogs.com/biopy/p/5768968.html